What is a Herniated Disc?
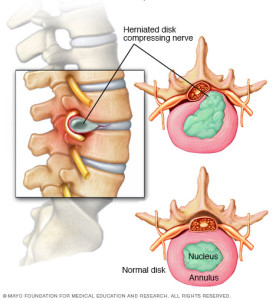
A herniated disc refers to a problem with one of the rubbery cushions (discs) between the individual bones (vertebrae) that stack up to make your spine.
A spinal disc is a little like a jelly donut, with a softer center encased within a tougher exterior. Sometimes called a slipped disc or a ruptured disc, a herniated disc occurs when some of the softer “jelly” pushes out through a crack in the tougher exterior.
A herniated disc can irritate nearby nerves and result in pain, numbness or weakness in an arm or leg. On the other hand, many people experience no symptoms from a herniated disc. Most people who have a herniated disc don’t need surgery to correct the problem.
You can have a herniated disc without knowing it — herniated discs sometimes show up on spinal images of people who have no symptoms of a disc problem. But some herniated discs can be painful. Most herniated discs occur in your lower back (lumbar spine), although they can also occur in your neck (cervical spine).
Dr Castillo is now offering lumbar and cervical braces to help treat back and neck pain. Click here to learn more
Symptoms
The most common signs and symptoms of a herniated disc are:
- Arm or leg pain. If your herniated disc is in your lower back, you’ll typically feel the most intense pain in your buttocks, thigh and calf. It may also involve part of the foot. If your herniated disc is in your neck, the pain will typically be most intense in the shoulder and arm. This pain may shoot into your arm or leg when you cough, sneeze or move your spine into certain positions.
- Numbness or tingling. People who have a herniated disc often experience numbness or tingling in the body part served by the affected nerves.
- Weakness. Muscles served by the affected nerves tend to weaken. This may cause you to stumble, or impair your ability to lift or hold items.
A herniated disc can irritate nearby nerves and result in pain, numbness or weakness in an arm or leg.
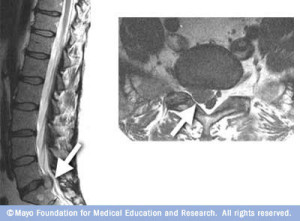
A MRI can be used to confirm the location of the herniated disc and to see which nerves are affected
What Causes Herniated Discs?
Disc herniation is most often the result of a gradual, aging-related wear and tear called disc degeneration. As you age, your spinal discs lose some of their water content. That makes them less flexible and more prone to tearing or rupturing with even a minor strain or twist.
Most people can’t pinpoint the exact cause of their herniated disc. Sometimes, using your back muscles instead of your leg and thigh muscles to lift large, heavy objects can lead to a herniated disc, as can twisting and turning while lifting. Rarely, a traumatic event such as a fall or a blow to the back can cause a herniated disc.
Factors that increase your risk of a herniated disc may include:
- Weight. Excess body weight causes extra stress on the discs in your lower back.
- Occupation. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways and twisting also may increase your risk of a herniated disc.
- Genetics. Some people inherit a predisposition to developing a herniated disc.
Complications with Herniated Discs
Your spinal cord doesn’t extend into the lower portion of your spinal canal. Just below your waist, the spinal cord separates into a group of long nerve roots (cauda equina) that resemble a horse’s tail. Rarely, disc herniation can compress the entire cauda equina. Emergency surgery may be required to avoid permanent weakness or paralysis.
Seek emergency medical attention if you have:
- Worsening symptoms. Pain, numbness or weakness may increase to the point that you can’t perform your usual daily activities.
- Bladder or bowel dysfunction. People who have the cauda equina syndrome may become incontinent or have difficulty urinating even with a full bladder.
- Saddle anesthesia. This progressive loss of sensation affects the areas that would touch a saddle — the inner thighs, back of legs and the area around the rectum.
Diagnosing Herniated Discs
During the physical exam, your doctor will check your back for tenderness. He or she may ask you to lie flat and move your legs into various positions to help determine the cause of your pain. Your doctor may also perform a neurological exam, to check your:
- Reflexes
- Muscle strength
- Walking ability
- Ability to feel light touches, pinpricks or vibration
In most cases of herniated disc, a physical exam and a medical history are all that’s needed to make a diagnosis. If your doctor suspects another condition or needs to see which nerves are affected, he or she may order one or more of the following tests.
Imaging tests
- X-rays. Plain X-rays don’t detect herniated discs, but they may be performed to rule out other causes of back pain, such as an infection, tumor, spinal alignment issues or a broken bone.
- Computerized tomography (CT scan). A CT scanner takes a series of X-rays from many different directions and then combines them to create cross-sectional images of your spinal column and the structures around it.
- Magnetic resonance imaging (MRI). Radio waves and a strong magnetic field are used to create images of your body’s internal structures. This test can be used to confirm the location of the herniated disc and to see which nerves are affected.
- Myelogram. A dye is injected into the spinal fluid, and then X-rays are taken. This test can show pressure on your spinal cord or nerves due to multiple herniated discs or other conditions.
Nerve tests
Electromyograms and nerve conduction studies measure how well electrical impulses are moving along nerve tissue. This can help pinpoint the location of the nerve damage.
 Skip to content
Skip to content
